Clear Your Backlog
Calvient is an AI Workflow Cockpit that orchestrates your crucial tasks—referrals, prior auths, document flows—so work moves from backlog to done and patients flow through the door smoothly.
Most AI promises the moon, then fizzles. Calvient is built by experienced healthcare engineers who know your workflows inside and out — automating referrals, faxes, and prior auths so your staff gets hours back every week.
See Calvient in action. We'll show you how it works for your practice.
Trusted by teams in healthcare









You know that person who knows everything and gets things done? Now give those same superpowers to your entire team. Start saving time now—humans and AI working together on your most vital patient workflows.
EHRs don't cut it. You need a toolset that actually helps you get work done. See how Calvient delivers a better experience with real results:.
Calvient is an AI Workflow Cockpit that orchestrates your crucial tasks—referrals, prior auths, document flows—so work moves from backlog to done and patients flow through the door smoothly.
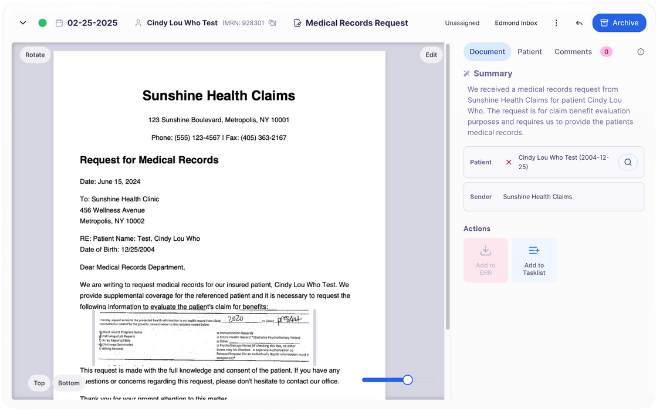
Turn minutes per document into seconds. Hours saved per week for every staff member with our Practice Inbox.
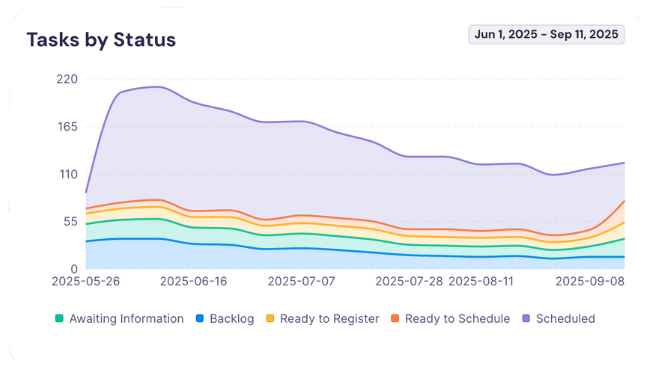
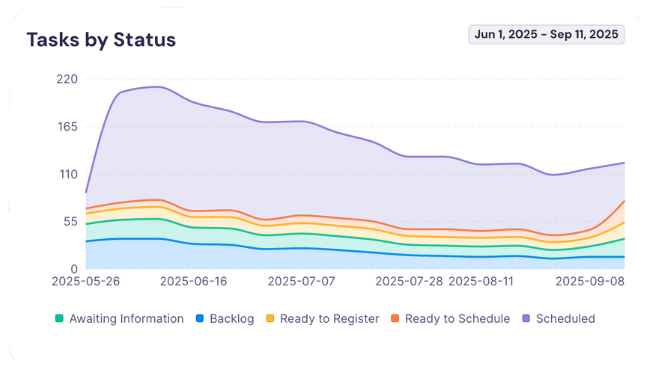
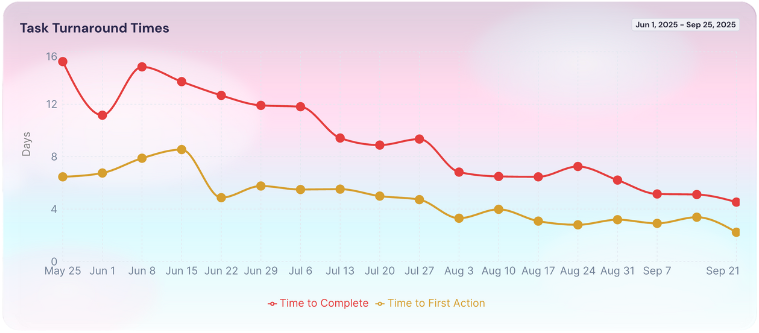
Track turnaround time and first contact speed for tasks such as prior authorizations, referrals, and medical record requests. Improve the metrics that show how much your team gets done.
Interoperability and speed with the EHRs you already use.
Practical automation with Practice Intelligence—safe, measurable, and built on a solid foundation.
Not just reporting—admins get granular control over access and assignment flows, down to the document type. Everything runs on rails in Calvient, while administrators keep multi‑team operations visible and smooth.
From specialty practices to health systems, teams choose Calvient to streamline their workflows.
"With their affordable and innovative approach to healthcare technology, Calvient is truly taking us into a better future of medicine."
.svg)
Stop the chaos of spreadsheets, sticky notes, and tasks scattered across systems. Our proven methodology brings order first, then speed, then intelligence.
Bring work together. Instead of monitor pinatas covered in sticky notes and EHR tasks that aren't really your job, Calvient centralizes workflows like prior authorizations, referrals, and medical record requests—giving you a measurable baseline.
Make staff faster. Our specialized tools help review high volumes quickly. Minutes turn into seconds so your team gets more done with the same effort, week after week.
Introduce Practice Intelligence. Now you're ready for our AI engine that takes tasks completely off the table. Automation that actually works because the foundation is solid.
See how teams like yours are getting 10–20% more productive in their first 90 days. Let's talk about your workflow challenges.
See Calvient in action. We'll show you how it works for your practice.